TMS Overview

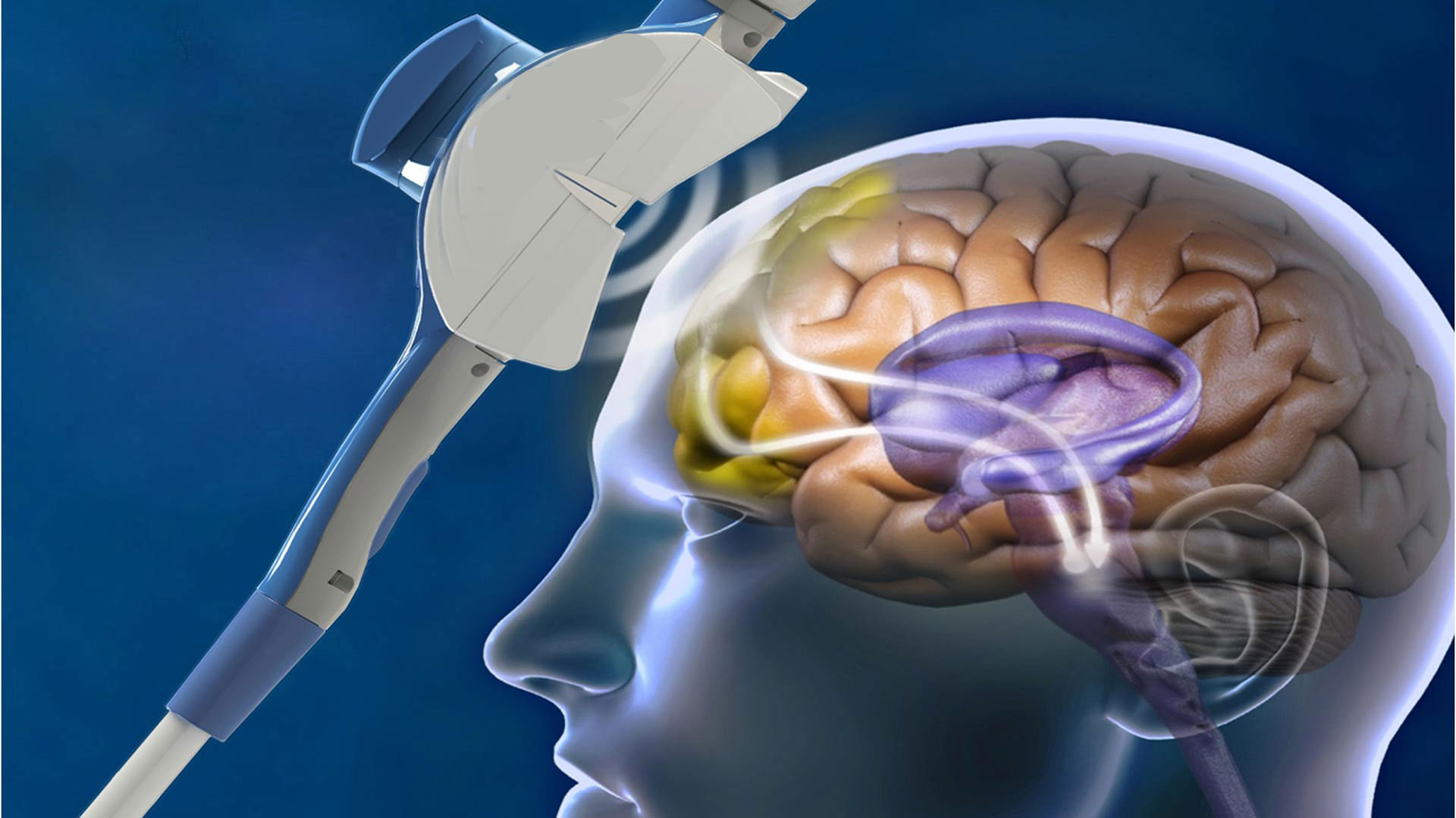
Does insurance cover tms – Transcranial Magnetic Stimulation (TMS) is a non-invasive brain stimulation technique that uses magnetic pulses to stimulate specific areas of the brain. It has emerged as a promising treatment option for various mental health conditions, particularly depression, anxiety, and obsessive-compulsive disorder (OCD).
TMS Therapy Types and Mechanisms of Action
Different types of TMS therapy target specific brain regions and employ different stimulation patterns to achieve therapeutic effects.
- Repetitive TMS (rTMS): This is the most commonly used type of TMS. It involves delivering repetitive magnetic pulses to a specific brain region, typically the dorsolateral prefrontal cortex (DLPFC), which is involved in mood regulation. rTMS can be applied in two ways:
- High-frequency rTMS: This type of stimulation is thought to increase neuronal activity in the target area, leading to an antidepressant effect.
- Low-frequency rTMS: This type of stimulation is thought to decrease neuronal activity, which may be beneficial for conditions like anxiety or OCD.
- Theta Burst Stimulation (TBS): This technique delivers bursts of magnetic pulses in a pattern that mimics the natural theta brainwave frequency. TBS is believed to be more effective than rTMS at inducing neuroplasticity, which is the brain’s ability to adapt and change.
- Intermittent Theta Burst Stimulation (iTBS): This type of TBS is used to enhance neuronal activity, similar to high-frequency rTMS.
- Continuous Theta Burst Stimulation (cTBS): This type of TBS is used to decrease neuronal activity, similar to low-frequency rTMS.
TMS Procedure
A TMS treatment session typically involves the following steps:
- Preparation: The patient will be seated comfortably in a chair. The therapist will place a magnetic coil over the patient’s head, targeting the specific brain region to be stimulated.
- Stimulation: The therapist will deliver magnetic pulses through the coil. The patient may feel a tapping sensation on their scalp.
- Monitoring: The therapist will monitor the patient’s response to the stimulation and adjust the treatment parameters as needed.
Each TMS session lasts for approximately 30 minutes. The frequency of treatment sessions varies depending on the individual patient and the condition being treated. For example, for depression, treatment sessions are typically given 5 days a week for 4-6 weeks.
Navigating Insurance Coverage
Understanding your insurance coverage for TMS therapy is crucial. Many insurance plans cover TMS, but the details can vary. This section will guide you through the process of verifying your coverage and navigating the billing process for TMS treatment.
Verifying Insurance Coverage
To determine if your insurance plan covers TMS therapy, contact your insurance provider directly. Ask specific questions to clarify your coverage, such as:
- Does my plan cover TMS therapy for my specific diagnosis?
- What is the coverage amount for TMS treatments?
- Are there any pre-authorization requirements?
- What is the co-pay or coinsurance for TMS therapy?
- Are there any specific providers or facilities within my network for TMS treatment?
Understanding the Billing Process
Once you have verified your coverage, it’s essential to understand how TMS therapy is billed to your insurance provider. The billing process usually involves the following steps:
- Pre-authorization:You may need to obtain pre-authorization from your insurance provider before starting TMS treatment. This involves submitting a request for coverage and receiving approval.
- Treatment:Once pre-authorization is approved, you can begin your TMS treatment sessions. The provider will bill your insurance company for each session.
- Claims processing:Your insurance provider will review the claims submitted by the provider and process them based on your coverage.
- Co-payment or coinsurance:You may be responsible for a co-payment or coinsurance for each treatment session.
- Out-of-pocket expenses:You may have out-of-pocket expenses for TMS therapy, such as deductibles or co-pays, depending on your insurance plan.
Obtaining Pre-authorization
Pre-authorization is a process where you request your insurance provider to approve coverage for TMS therapy before you start treatment. This step is crucial to ensure that your treatment is covered by your insurance plan. Here’s a step-by-step guide to obtaining pre-authorization:
- Contact your insurance provider:Call your insurance provider and inform them that you are seeking pre-authorization for TMS therapy.
- Gather necessary information:Collect all the necessary information required for pre-authorization, such as your insurance card details, diagnosis, and physician’s contact information.
- Submit a pre-authorization request:Your physician or the TMS clinic will submit a pre-authorization request to your insurance provider.
- Review the pre-authorization decision:Once the insurance provider reviews the request, they will notify you of their decision.
- Appeal if necessary:If your pre-authorization is denied, you can appeal the decision.
Insurance Claim Process for TMS Treatments, Does insurance cover tms
The following table Artikels the common steps involved in the insurance claim process for TMS treatments:
| Step | Description |
|---|---|
| 1. Treatment | You receive TMS treatment sessions from a qualified provider. |
| 2. Billing | The provider submits claims to your insurance company for each treatment session. |
| 3. Claims processing | Your insurance company reviews the claims and processes them based on your coverage. |
| 4. Payment | Your insurance company pays the provider directly, and you may be responsible for co-payments or coinsurance. |
| 5. Explanation of benefits (EOB) | You will receive an EOB from your insurance company outlining the claims processed, payments made, and your remaining out-of-pocket expenses. |
Popular Questions: Does Insurance Cover Tms
How does TMS work?
TMS uses magnetic pulses to stimulate specific areas of the brain, aiming to regulate brain activity and improve symptoms. The therapy is non-invasive and typically involves daily sessions over several weeks.
What are the side effects of TMS?
Common side effects of TMS are mild and temporary, such as headaches, scalp discomfort, and lightheadedness. More serious side effects are rare.
Is TMS covered by Medicare?
Medicare coverage for TMS varies depending on the specific plan and individual circumstances. It’s essential to contact Medicare directly for clarification.
What are some alternative payment options for TMS?
Alternative options include financing plans, out-of-pocket payments, and charitable organizations. Researching available resources is crucial.